Summer is Here: Part 2!
More summer rashes this week!
By Marie Leger, MD PhD
Polymorphous light eruption, or PMLE for short. Colloquially, this could be described as a kind of sun allergy–and both UVA and UVB rays can be responsible. It is more common in young women, usually occurs in the spring or early summer, and classically appears a day or two after sun exposure. It can look variable, hence the name. I’ve seen blisters, symmetric bumps on sun exposed areas, mosquito bite-like rashes, and other presentations. In Black and Asian patients, it has been described as pinpoint sized bumps in sun exposed areas, and in multiple patients from Central and South America, I have seen tiny, itchy bumps after sun exposure on the backs of hands. With continued sun exposure, the rash often disappears—and people are often better by the end of the summer for this reason. Dermatologists call this “skin hardening” but your skin doesn’t really get hard (We do sometimes use controlled light exposure to manage it though). Other things can mimic this rash—drug allergies, lupus, and porphyrias for example--so if you get red or itchy after sun exposure, it’s worth seeing your dermatologist to figure out what is going on. Sometimes PMLE persists for years, but it often gets better with time.
Flagellate dermatitis. This is not really a summer rash, but I’m including it here because I saw a patient with it recently. A classic board exam question for budding dermatologists would include a photo of someone’s back with a slew of linear welts on their skin. “What did this patient eat?” The answer—raw shitake mushrooms. The rash is caused by a toxic reaction to the polysaccharide lentinan in raw, powdered, or undercooked shitakes and it is more common in places where more of these mushrooms are consumed (for example, China and Japan). New York is also a shitake mushroom-loving city, but I’ve only seen it twice in my whole ten years as a dermatologist here. It is itchy and very impressive looking (google “flagellate dermatitis” and “shitake” and you will see what I mean) and usually goes away on its own in a week or two—but it can last up to two months. This poetic rash lends itself to a haiku.
Sumptuous mushroom.
Shitake I’ll eat you raw.
Sleepless itchy nights.
Treatment consists of waiting it out and antihistamines.
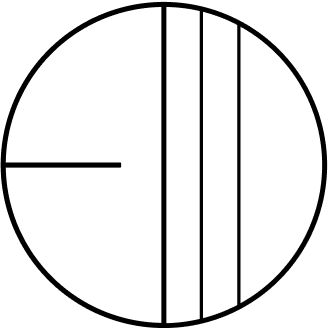
Erythema migrans. Ticks are out in full force during the summer months. I recently found a nymph on my dog and the illustrator of this blog had one on his leg after a recent hike. Once I saw a patient with a “new mole” that had been on his back for several weeks and when I examined it closely it was moving. The Ixodes tick—on my patient, my dog, and the artist-- is responsible for Lyme disease--which can transmit the causal bacteria (Borrelia burgdorferi in the US) via a bite. It’s not just your imagination that there is more Lyme disease around these days. Since it became a reportable (and trackable) condition in the US in the 1990s, cases have continued to go up and expand geographically due to climate change and changing land use practices. More deer and more ticks means more Lyme in more places. Actually, it’s not fair to just blame the deer—these ticks also like chipmunks, mice, birds, dogs, and shrews. There is a characteristic rash—described as a bulls eye rash—that develops at the site of the tick bite in most (60-90%) people who get Lyme disease, usually in the first few days to weeks after a tick bite. Even though there is a blood test for Lyme titers, the first weeks after exposure tests are often negative—so when we see patients with a convincing history and a characteristic rash we just treat for Lyme.